For people diagnosed with neuroendocrine tumors (NETs), treatment has historically been shown to prevent disease development. However, there have been no available treatments that have reduced these tumors – so far.
Doctors are now treating some forms of this cancer in neuroendocrine cells with a new radiation-based treatment. This has shown impressive effectiveness in reducing NETs, even if it has spread to other areas.
In this article, we provide all the details of the neuroendocrine tumour.
What is the Neuroendocrine Tumor?
Neuroendocrine tumors are cancers that begin with specialized cells called neuroendocrine cells. They have properties similar to those of nerve cells and hormone-producing cells.
Neuroendocrine tumours are rare and can appear anywhere in the body. Some neuroendocrine tumours occur in the lungs, appendix, small intestine, rectum, and pancreas.
There are a variety of forms of neuroendocrine tumours. Some of them grow slowly, and some grow very fast. Some neuroendocrine tumours induce excess hormones (functional neuroendocrine tumours). Others do not produce hormones or release sufficiently to cause symptoms (nonfunctional neuroendocrine tumours).
The diagnosis and treatment of neuroendocrine tumours depend on:
- The type of tumour
- Its position
- Whether it produces excess hormones
- How dangerous it is
- And if it has spread to other areas of the body
Types of neuroendocrine tumours
Neuroendocrine tumours often occur in organs such as the liver, small intestine, colon, rectum.
There are several types of NETs available, including:
- Functional, meaning that hormones are produced
- Nonfunctional, non-producing hormones
Symptoms
Neuroendocrine tumors do not always cause signs and symptoms at first. But, the symptoms you may experience depend on the position of your tumour and whether it releases excess hormones.
In general, the signs and symptoms of neuroendocrine tumours can include:
- The pain of a growing tumour
- A growing lump that you can feel under your skin
- Felt unusually tired
- Losing weight without trying to do so
Neuroendocrine tumours that contain excess hormones (functional tumours) may be the cause:
- Skin flushing
- Diarrhoea
- Frequent urination
- Increased thirst
- Dizziness
- Shakiness
- Skin rash
Causes
The exact cause of neuroendocrine tumors is not clear. These cancers begin in neuroendocrine cells. These cancer cells have similar characteristics to those of nerve cells and hormone-producing cells. Neuroendocrine cells are present all over the body.
Neuroendocrine tumors begin when neuroendocrine cells produce changes (mutations) in their DNA. But the DNA inside the cell provides instructions to tell the cell what to do. Hence, the changes tell the neuroendocrine cells to multiply quickly and form a tumor.
Some neuroendocrine tumors are growing very slowly. Others are active tumors that invade and damage normal body tissues or spread (metastasize) to other areas of the body.
Risk factors
The risk of neuroendocrine tumors is higher in people who inherit genetic syndromes that increase cancer risk. Examples include:
- Multiple endocrine neoplasias, type 1 (MEN 1)
- Multiple endocrine neoplasias, type 2 (MEN 2)
- Von Hippel-Lindau disease
- Tuberous sclerosis
- Neurofibromatosis
Diagnosis
Testing and treatments that may be used to diagnose a neuroendocrine tumour may depend on where the tumour is located in the body. In general, the tests may include:
- Physical exam. Your doctor may examine your body to understand your signs and symptoms better. They may feel for swollen lymph nodes or look for signs that a tumor produces excess hormones.
- Tests to look for excess hormones. Your doctor may recommend testing your blood or urine. These tests search for symptoms of excessive hormones that neuroendocrine tumors cause.
- Imaging tests. You may have to undergo imaging scans, such as ultrasound, CT, and MRI, to create photos of the tumor. Also, pictures for neuroendocrine tumors are sometimes developed using positron emission tomography (PET).
- Procedures to remove a sample of cells for testing (biopsy). The doctor may insert a long, thin tube with a light and a camera at the end of your cells into your lungs (bronchoscopy), your esophagus (endoscopy), or your rectum (colonoscopy), depending on your condition. Sometimes extracting a tissue sample may require surgery.
Suppose there is a risk that your neuroendocrine tumour may have spread to other areas of the body. Then additional tests may be required to determine cancer’s extent.
Treatment
The treatment choices for your neuroendocrine tumour will depend on the type of tumour and its location. It also depends on whether there are signs and symptoms of excess hormones.
In general, treatment options for neuroendocrine tumours may include:
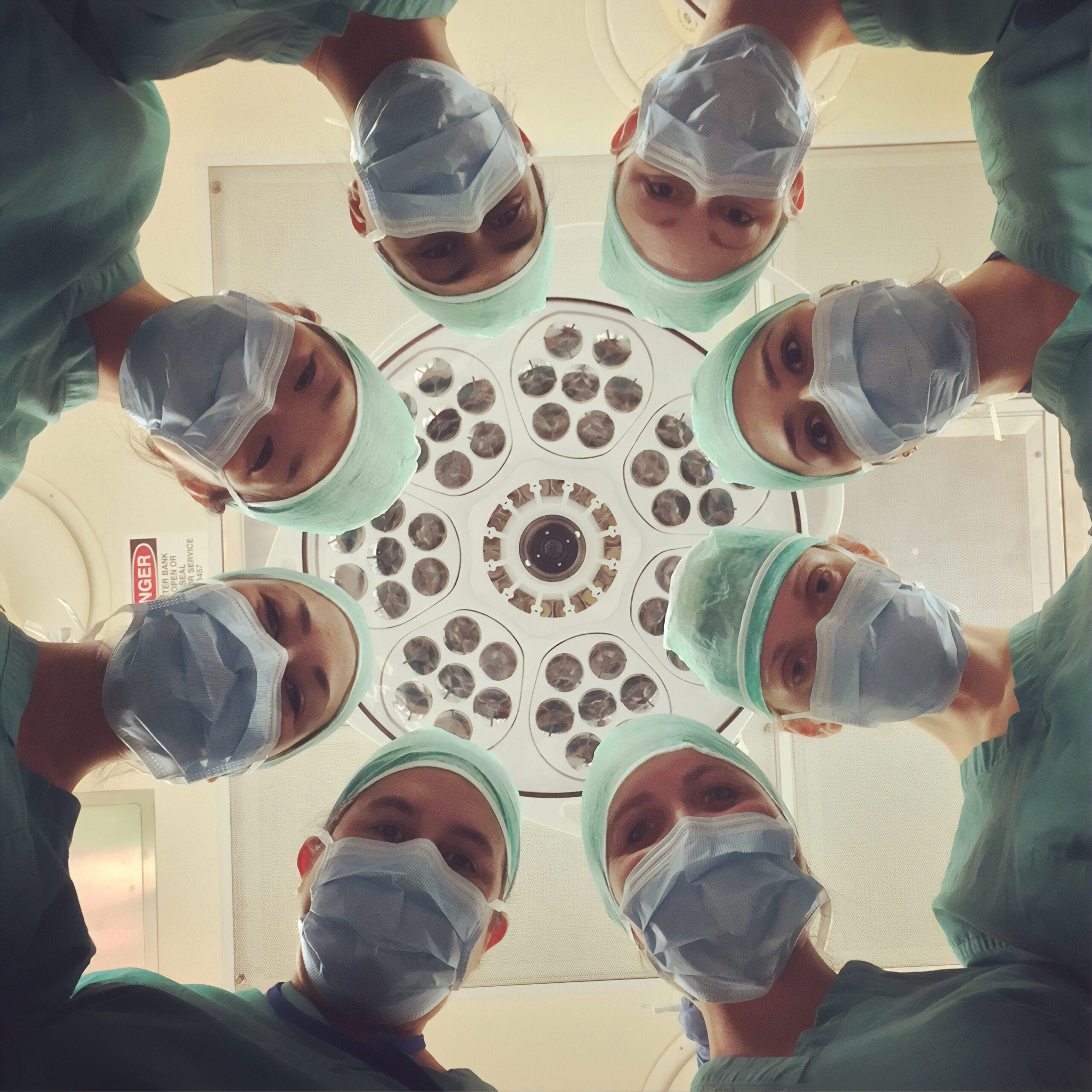
- Surgery. Doctors use surgery for the removal of the tumor. Where possible, surgeons will remove the whole tumor and some of the healthy tissue surrounding it. If doctors can not remove the tumor entirely, it will help remove as much of it as possible.
- Chemotherapy. Chemotherapy uses strong medications to kill tumor cells. Doctors can give it through a vein in your arm, or you can take it as a pill. He can also prescribe chemotherapy if there is a risk that the neuroendocrine tumor may recur after surgery. Doctors also use it for advanced tumors that they cannot by surgery.
- Targeted drug therapy. Targeted drug treatment works on specific abnormalities of tumor cells. By blocking the abnormalities, Targeted drug treatments may cause tumor cells to die. Targeted drug treatment is usually combined with advanced neuroendocrine tumor chemotherapy.
- Radionuclide receptor peptide therapy (PRRT). PRRT combines a drug attacking cancer cells with a small amount of radioactive substance. It allows the radiation to be transferred directly to cancer cells. Doctors use the PRRT drug, lutetium Lu 177 dotatate (Lutathera), to treat advanced neuroendocrine tumors.
- Medications to control excess hormones. Suppose your neuroendocrine tumor releases extra hormones. Then your doctor may recommend taking medicine to control your signs and symptoms.
- Radiation therapy. Radiotherapy uses powerful energy beams, such as x-rays and protons, to destroy tumor cells. Hence, some types of neuroendocrine tumors can respond to radiation therapy. Doctors recommend it if surgery is not an option.
Other treatments may be available to you depending on your particular condition.
Coping and support
The diagnosis of a neuroendocrine tumour can be stressful and frustrating. With time, you will learn ways to deal with distress and uncertainty. Before then, you may find that it helps:
- Learn enough about your diagnosis to make your treatment options. Ask the doctor if you have a neuroendocrine tumor, including your medical plans and your prognosis, if you like. Learn more about the nature of the neuroendocrine tumor you have. Then you can become more confident in making treatment decisions.
- Turn to help family and friends. Keep close to your family and friends for support. It can be hard to talk about your condition because you’re sure to have several reactions when you share the story. But talking about your diagnosis and passing on details about your cancer can help you deal with it.
- Connect with other neuroendocrine tumors. Try joining a support group, either in the neighbourhood or on the internet. A support group of individuals with the same diagnosis may be a source of useful information. They can also provide constructive advice and encouragement.
The Bottom Line
You should do a few things from diet to exercise to taping into a healthy support network to make you feel better when you have neuroendocrine tumours (NET). Everything depends on where the tumour is and the type of signs it causes.
No matter the priority, lifestyle changes can take a long way to keep your mind and body healthy.
.