Bedwetting is an unintentional release of urine during sleep. It is a concern if the child is over 7 years of age and continues to wet the bed for two or more days a week for three months in a row. And, you may treat it by changing the behavior of the child or by using different medications.
What is bedwetting?
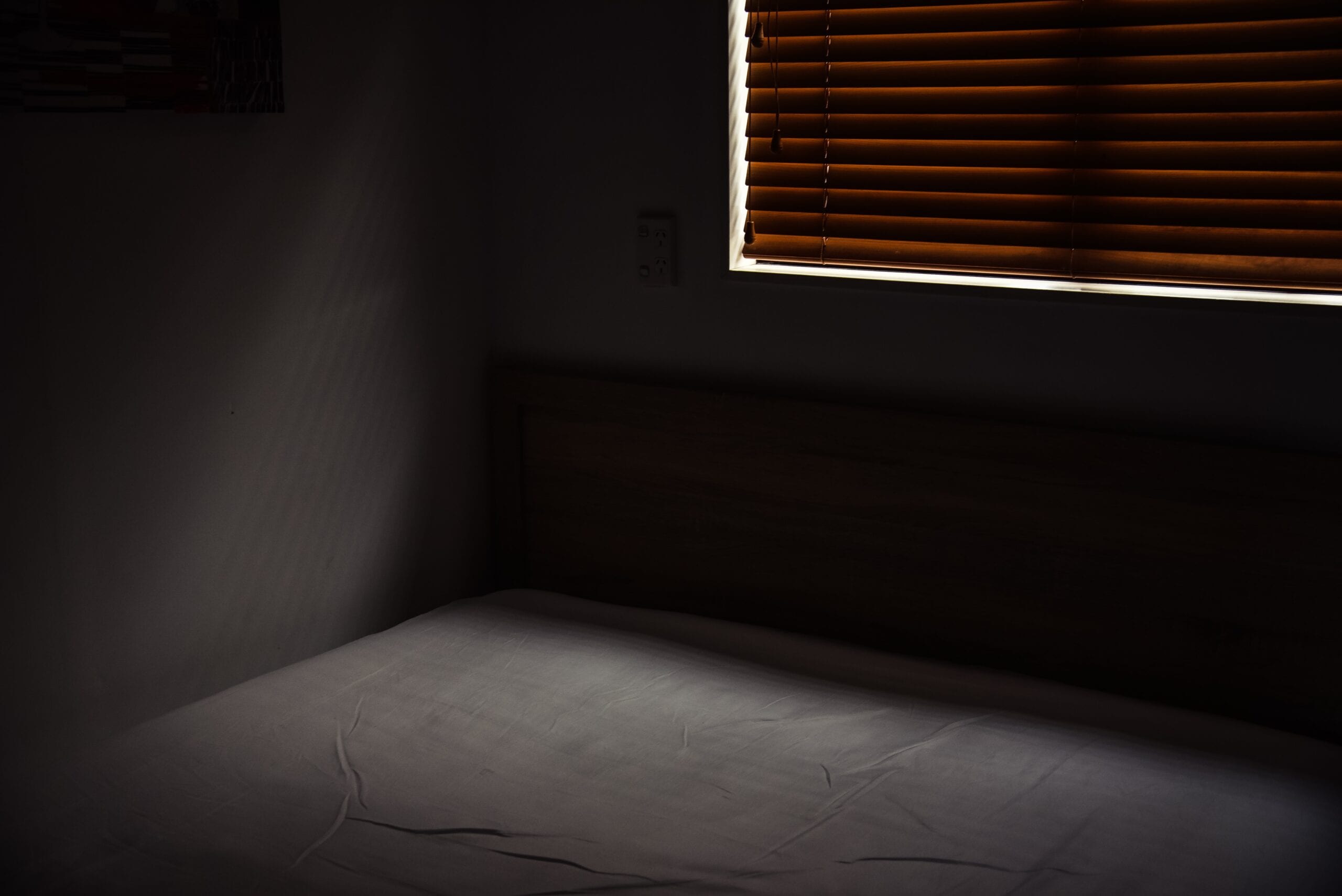
Bedwetting, also known as nocturnal enuresis, is the involuntary or unintentional release of urine during sleep. Even after toilet training, bedwetting is a common issue among children.
Many children will gradually stop wetting the bed on their own as they get older. Usually, children stop wetting their beds between 3 and 5 years of age.
While bedwetting is not a serious condition, it can bring stress to the child and the family. Children who wet their beds may feel ashamed or embarrassed. They might stop taking part in activities, such as sleeping or camping because they are afraid that they might wet the bed when they’re away from home.
Are there multiple types of bedwetting?
Yes. There are two major types of bedwetting—primary and secondary nocturnal enuresis:
- Primary nocturnal enuresis is a condition in which the person has never stayed dry for six months in a row or longer during the night.
- Secondary nocturnal enuresis is a disorder in which the child has begun to wet the bed again after not wetting it for six months or longer. Secondary enuresis is more likely to be due to a medical or neurological disorder.
Causes
No one knows exactly what causes bedwetting, but a variety of factors can play a role:A small bladder. Your child’s bladder can not grow enough to hold the urine produced during the night.
Inability to recognize a full bladder. If the nerves regulating the bladder are slow to develop, a full bladder can not wake your child—especially if your child is a deep sleeper.
The hormonal imbalance. Some children do not produce enough anti-diuretic hormone (ADH) to slow down their night-time urine production during childhood.
Urinary tract infection. This infection will make it difficult for your child to control their urine. Signs and symptoms can include bedwetting, daytime spills, frequent urination, red or pink urine, and urinary pain.
Sleep apnea. Bedwetting is also a sign of obstructive sleep apnea, a condition in which the child’s breathing is disrupted at sleep—often caused by enlarged or damaged tonsils or adenoids. Other signs and symptoms can include snoring and drowsiness throughout the day.
Diabetes. Bedwetting can be the first symptom of diabetes for a child who is usually dry at night. Other signs and symptoms can include passing large amounts of urine at once, excessive thirst, exhaustion, and weight loss despite a healthy appetite.
Chronic constipation. The same muscles that control the elimination stools control the urine as well. When constipation is long-term, these muscles may become unstable and lead to bedwetting at night.
Structural defects in the urinary tract or nervous system. Bedwetting is rarely associated with a defect in the child’s neurobiology or urinary system.
Risk factors
Bedwetting can affect anyone, but it’s twice as common in boys as it is in girls. Several causes are associated with an increased risk of bed-wetting, including:
- Stress and fear. Stressful events—like being a big brother or sister, beginning a new school, or sleeping away from home—may cause a wet bed.
- Family history. If one or more of the child’s parents wet the bed as children, their child often has a significant risk of wetting the bed.
- Attention to deficiency/hyperactivity disorder (ADHD). Bedwetting is more likely in children with ADHD.
Diagnosis:
Depending on the situation, the following may be prescribed by your doctor to identify any underlying cause of bedwetting and to help determine treatment:
- Physical test
- Discussion of symptoms, fluid consumption, family history, bowel, and urinary habits, and issues associated with bedwetting;
- Urine tests to check for effects of infection or diabetes
- X-rays or other imaging tests of the kidneys or bladder to analyze the structure of the urinary tract;
- Other forms of tests or assessments of the urinary tract as required
Treatment
Most of those children grew up bedwetting on their own. If you need treatment then you should discuss solutions with your doctor and identify what would work better with your situation.
Suppose your child is not especially disturbed or embarrassed by an occasional wet night. In that case, lifestyle changes—such as eliminating coffee entirely and restricting the intake of fluid in the evening—may work well. However, if lifestyle changes are not effective, or if your high school student is scared to wet the bed. Additional treatments can improve him or her.
If identified, the underlying causes of bedwetting, such as constipation or sleep apnea, should be addressed before further treatment.
Options for the treatment of bedwetting can include moisture alarms and medication.
Medication
Your child’s doctor can recommend medicine for a short period of time to stop bedwetting as a last resort.
Certain types of medication may:
- Slow production of urine during the night. Drug desmopressin (DDAVP) decreases the production of urine at night. But drinking too much liquid with the drug can cause problems. You should stop desmopressin if your child has symptoms such as fever, diarrhea, or nausea. Make sure to follow the instructions carefully for the use of this drug.
- Desmopressin is taken orally as a tablet and is only for children above 5 years of age. According to the Food and Drug Administration, nasal spray forms of desmopressin (Noctiva, others) are no longer recommended for bedwetting due to the possibility of severe side effects.
- Calm your bladder. If your child has a small bladder, an anticholinergic medication such as oxybutynin (Ditropan XL) can help reduce the bladder’s contraction and increase the capacity of the bladder, especially if there is daytime wetting. This medication may usually be given combined with other drugs. You should only use this drug when all therapies have failed.
- Sometimes a mixture of drugs is more effective. There are no guarantees, however, and the drug does not solve the problem. Bedwetting normally resumes when you stop the drug until it resolves on its own at an age that varies from child to child.
The Bottom Line
It might not be possible to avoid all enuresis cases, especially those related to the baby’s anatomy problems. It may help reduce the disease’s problems when your child is evaluated by a pediatrician as soon as symptoms appear. Being positive and patient with a child during toilet training will help prevent negative feelings about using the toilet.